Intrauterine Insemination Saudi Arabia and Intrauterine Insemination Kuwait Price Comparison: A Comprehensive Overview

Intrauterine insemination (IUI) has become a popular fertility treatment in many countries, including Saudi Arabia and Kuwait. Comparing the prices of IUI treatments between these two nations can help prospective patients make informed decisions about their fertility healthcare options. Saudi Arabia and Kuwait offer modern medical facilities and experienced specialists in reproductive health, but the costs vary significantly.
Saudi Arabia boasts advanced fertility clinics, often with competitive pricing due to the larger number of healthcare providers. Kuwait, on the other hand, may have fewer clinics but offers personalised care and shorter waiting times. Patients in both countries benefit from exceptional medical services, but understanding the price differences can be crucial when planning treatment.
The cost of IUI in Saudi Arabia typically ranges from £500 to £1,000 per cycle, whereas in Kuwait, it might range from £700 to £1,200. These figures highlight that choosing the right country for IUI treatments can involve a trade-off between cost and potential waiting periods. Comparing these prices allows individuals to weigh their options and select the best possible route for their fertility journey.
Understanding Intrauterine Insemination
Intrauterine insemination (IUI) is a common procedure used to treat various types of infertility. Specifically, it can address issues related to male factor infertility, unexplained infertility, and mild female factor infertility.
Fundamentals of IUI
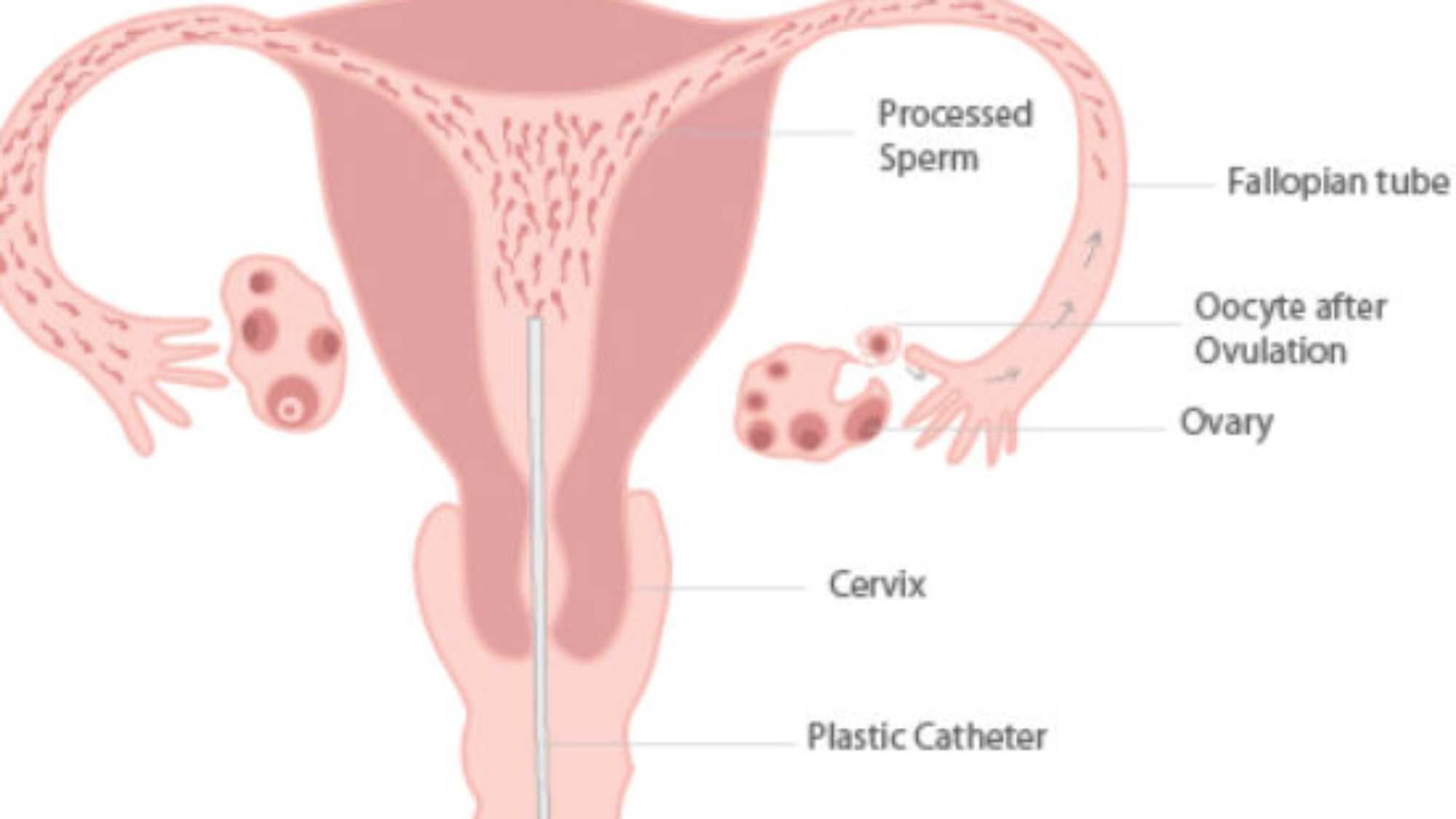
Intrauterine insemination involves placing sperm directly into a woman’s uterus during ovulation. This process increases the number of sperm that reach the fallopian tubes. It is often recommended for couples facing challenges such as mild male factor infertility or unexplained infertility.
The procedure involves several steps: stimulating the ovaries with medication, monitoring ovulation through ultrasound, and introducing the prepared sperm into the uterus using a thin catheter. This method enhances the likelihood of the sperm meeting the egg, thus promoting fertilisation.
IUI Versus IVF Procedures
IUI and in vitro fertilisation (IVF) are both assisted reproductive technologies but differ significantly. While IUI involves direct sperm introduction into the uterus, IVF includes harvesting eggs, fertilising them outside the body, and then implanting the embryos back into the uterus.
IUI is less invasive and typically more affordable compared to IVF. It is ideal for those with mild fertility issues. IVF, on the other hand, is suitable for severe infertility problems, including blocked fallopian tubes or severe male factor infertility. IVF offers higher success rates but comes with increased costs and complexity.
Role of Age in IUI Success
Age plays a crucial role in the success rates of IUI. Generally, women under 35 experience higher success rates, as fertility naturally declines with age. For instance, the success rate for women under 35 ranges from 10% to 20% per cycle, whereas it drops significantly for women over 40.
Younger women typically have healthier eggs, which enhances the chances of conception. Conversely, older women may face diminished ovarian reserve or egg quality, impacting the effectiveness of IUI. Thus, age is a critical factor in determining the appropriateness and potential success of IUI in fertility treatments.
Indications for IUI in Fertility Treatment
Intrauterine insemination (IUI) is often used to enhance the chances of pregnancy in couples facing specific fertility issues. Key situations where IUI is recommended include unexplained infertility and mild male factor infertility.
Unexplained Infertility
Unexplained infertility refers to situations where fertility tests fail to identify a clear cause for a couple’s inability to conceive. For these couples, IUI can be a practical fertility treatment option.
During the procedure, sperm is directly placed into the uterus, potentially increasing the chances of successful fertilisation. This bypasses potential issues related to cervical mucus or minor sperm motility problems. Clinical pregnancy rates for this group can improve, especially when combined with ovarian stimulation.
Mild Male Factor Infertility
Mild male factor infertility includes conditions where sperm count or motility is slightly below normal but not severely impaired. IUI can benefit these couples by concentrating and placing the sperm closer to the egg.
This method helps in overcoming slight deficits in sperm quality. Using IUI, sperm washing is performed to enhance sperm quality, potentially increasing clinical pregnancy rates. Timed with ovulation, this method can significantly aid couples with mild male factor issues in achieving a successful pregnancy.
Comparative Analysis of IUI Costs
The costs of intrauterine insemination (IUI) in Saudi Arabia and Kuwait vary due to several factors, including healthcare systems, costing methods, and cost components. This section breaks down these differences to provide clear insights.
Cost Differences in Saudi Arabia and Kuwait
In Saudi Arabia, IUI procedures in private hospitals can range from SAR 3,000 to SAR 6,000. This variation depends on factors like the hospital’s reputation, location, and included services.
In contrast, Kuwait’s IUI costs range from KWD 600 to KWD 1,200 in private settings. Differences are influenced by similar factors, including whether medications and consultations are bundled. Comparing these costs reveals that treatments in Kuwait tend to be more expensive, but offer potentially more comprehensive services.
Activity-Based and Step-Down Costing
Activity-Based Costing (ABC) involves assigning costs to specific activities related to IUI, such as laboratory tests, medications, and clinical consultations. This method gives a more accurate picture of the true cost of each activity, aiding in precise budgeting and cost control.
Step-Down Costing allocates indirect costs to direct costs systematically. For instance, administrative expenses and facility overheads are assigned to clinical services. This costing method is crucial for understanding the full financial burden of IUI procedures and identifying areas where cost efficiencies can be implemented.
Cost Components: Direct and Indirect
Direct Costs include fees for consultations, medications, and the procedure itself. In both countries, these are the most visible and predictable expenses. Medication costs can vary significantly and often constitute a large portion of direct costs.
Indirect Costs cover administrative expenses, facility maintenance, and supportive services such as counselling. These costs, although not immediately apparent, contribute substantially to the overall expense of IUI treatments. Indirect costs can fluctuate based on factors like technology utilisation and hospital infrastructure, affecting the total pricing in both Saudi Arabia and Kuwait.
Clinical Outcomes of IUI
Intrauterine insemination (IUI) is often evaluated based on specific clinical outcomes such as pregnancy rates and live birth rates. These metrics provide insights into the effectiveness and success of the procedure.
Pregnancy Rates
Pregnancy rates for IUI can vary greatly depending on several factors including age, fertility health, and the use of fertility drugs. Studies show that women under 35 have higher success rates.
Clinical pregnancy is typically confirmed via ultrasound around four to six weeks after insemination. Reports from Cochrane reviews suggest an average clinical pregnancy rate from IUI of around 10-20% per cycle. This rate can increase with repeated cycles and optimal conditions.
Miscarriages do occur and their incidence is similar to that of natural conception. Success rates are reported as higher when fertility drugs are used in conjunction with IUI.
Live Birth Rates
Live birth rates are a crucial indicator of IUI’s success. These rates tend to be slightly lower than clinical pregnancy rates due to the possibility of miscarriage. Research indicates that live birth rates for women undergoing IUI range between 8-15% per cycle.
Factors such as maternal age and sperm quality significantly influence live birth rates. The use of controlled ovarian hyperstimulation can improve outcomes. Cochrane reviews and other studies consistently highlight the importance of these factors in achieving successful live births.
Recent data from clinics in Saudi Arabia and Kuwait might reflect similar trends, though local variations can occur. Reliable data form the basis of patient counselling and decision-making in fertility treatments.
Techniques Enhancing IUI Efficacy
Advancements in intrauterine insemination (IUI) focus on improving clinical pregnancy rates through specific techniques. These include endometrial injury and precise ovarian stimulation protocols to increase success rates.
Endometrial Injury
Endometrial injury, also known as endometrial scratching, is a procedure that involves intentionally causing minor damage to the endometrial lining. This technique is believed to promote an inflammatory response that can enhance embryo implantation. Studies indicate that performing endometrial injury in the cycle prior to IUI may improve clinical pregnancy rates.
During the procedure, a thin catheter is used to scratch the endometrial tissue. This is generally done mid-cycle, a few days before ovulation. Although the exact mechanism is not fully understood, it is thought that the injury may increase blood flow and growth factors in the endometrium, making it more receptive to implantation. Clinical trials have shown varying degrees of success, but this technique remains a valuable consideration for enhancing IUI outcomes.
Ovarian Stimulation Protocols
Ovarian stimulation is a critical component of IUI, aimed at inducing the development of multiple follicles to increase the chances of fertilisation. Two primary medications are used: Clomiphene Citrate and Gonadotrophins. Clomiphene Citrate is administered orally and works by blocking oestrogen receptors, tricking the brain into producing more follicle-stimulating hormone (FSH). This induces ovulation in women who do not ovulate regularly.
On the other hand, gonadotrophins are injectable hormones that directly stimulate the ovaries to produce multiple follicles. They are often used in cases of unexplained infertility or when Clomiphene Citrate alone is insufficient. Monitoring through ultrasound and blood tests is essential to adjust dosages and minimise the risk of ovarian hyperstimulation syndrome (OHSS). Proper protocol selection is crucial, as tailored stimulation can significantly affect clinical pregnancy rates in IUI procedures.
Financial Assessment Methods
Assessing the financial aspects of intrauterine insemination (IUI) treatments in Saudi Arabia and Kuwait involves a detailed evaluation of cost-effectiveness and sensitivity to probabilistic variables, focusing on the economic implications.
Cost-Effectiveness Analysis
Cost-Effectiveness Analysis (CEA) involves comparing the costs and health outcomes of different IUI treatments. This method helps determine the most efficient use of limited healthcare resources.
In Saudi Arabia, IUI costs can range from 2,500 to 5,000 SAR, while in Kuwait, the costs might be between 200 to 400 KWD. These costs are examined relative to the success rates of the procedures. Economists use Incremental Cost-Effectiveness Ratios (ICERs) to measure the additional cost per additional unit of health gain, typically in terms of Quality-Adjusted Life Years (QALYs).
A societal perspective is often adopted in CEA to capture the broad impacts, including non-direct costs such as lost productivity due to infertility treatments. By understanding the total economic impact, healthcare systems can optimise budget allocation. Both direct medical costs and indirect costs form a comprehensive view of the economic due diligence needed for policy decisions.
Probabilistic Sensitivity Analysis
Probabilistic Sensitivity Analysis (PSA) assesses the robustness of the cost-effectiveness results by incorporating variability and uncertainty in model parameters. This method uses statistical techniques to simulate a wide range of possible outcomes and their probabilities.
PSA helps policy-makers and clinicians in Saudi Arabia and Kuwait understand the likelihood that an IUI treatment will be cost-effective under various circumstances. Factors such as age, underlying fertility issues, and treatment protocols can influence these probabilities. Analyses are often conducted using Monte Carlo simulations to generate a distribution of possible results, thus offering a more nuanced understanding of economic viability.
By incorporating PSA, stakeholders can make more informed decisions that account for economic uncertainties, ensuring that resources are used in a way that offers the best potential outcomes for patients.
Risks and Complications of IUI
Intrauterine insemination (IUI) has its risks and complications, such as the chance of multiple pregnancies and the incidence of miscarriage. These factors warrant careful consideration when opting for this fertility treatment.
Multiple Pregnancies
One significant risk of IUI is the increased likelihood of multiple pregnancies. Unlike natural cycles, IUI often involves ovarian stimulation, which can result in the development of multiple follicles. This raises the probability of conceiving twins, triplets, or even higher-order multiples. Multiple pregnancies are associated with higher risks, including preterm birth, low birth weight, and complications for the mother, such as gestational diabetes and preeclampsia. Proper monitoring and tailored medication dosages are crucial to mitigate this risk.
Miscarriage Incidence
Another concern is the risk of miscarriage, which varies depending on individual health factors and the specifics of the IUI procedure. While IUI can increase the chance of conception, it does not eliminate the inherent risks of pregnancy, including miscarriage. The risk may be slightly higher in stimulated cycles compared to natural cycles, primarily due to the associated hormonal treatments. Close monitoring by a fertility specialist is essential to address any potential issues promptly.
Statistical Evaluation and Research
The statistical evaluation of intrauterine insemination (IUI) in Saudi Arabia and Kuwait focuses on clinical pregnancy rates, live birth rates, and results from randomised controlled trials. Public health perspectives and specific epidemiological data are also considered to provide a comprehensive understanding.
Epidemiology and Public Health
Epidemiological studies in Saudi Arabia and Kuwait highlight significant public health issues related to infertility treatment accessibility. Understanding regional differences in IUI utilisation is key.
Saudi Arabia has a higher frequency of infertility cases reported in urban versus rural areas. The public health strategies often focus on integrating IUI treatments within national health policies to improve access.
Kuwait’s public health initiatives are aimed at both increasing awareness and providing subsidised fertility treatments. Efforts include national campaigns to educate about infertility and available treatments.
Randomised Controlled Trials (RCTs)
Randomised controlled trials offer insights into the effectiveness of IUI in varying populations. RCTs from Saudi Arabia have examined clinical pregnancy rates and live birth rates, providing precise confidence intervals to ensure reliability.
Recent RCTs in Kuwait focus on comparing IUI success rates with other ART (assisted reproductive technology) methods. A key finding is that the clinical pregnancy rate for IUI ranges between 10% to 20% per cycle.
The importance of local RCTs cannot be overstated, as they provide region-specific success rates, guiding both patients and healthcare providers. These studies help in establishing standard protocols to ensure high-quality care across different settings.
Health Economics in Reproductive Medicine
Health economics in reproductive medicine assesses value, efficiency, and cost-effectiveness in fertility treatments such as intrauterine insemination (IUI). Pharmacoeconomics evaluates the economic impact of pharmaceuticals used in these treatments.
Pharmacoeconomics of Fertility Treatments
Pharmacoeconomics plays a crucial role in analysing the costs and financial outcomes associated with fertility drugs. Medication expenses can significantly affect the overall cost of treatments like IUI.
For instance, gonadotropins often used to stimulate ovulation can be expensive. Analysing the cost versus success rates helps to determine economically feasible treatment plans for patients.
Health economists use cost-effectiveness analysis to ensure that resources are optimally allocated. This involves comparing various medications and their impacts to provide financially viable and effective treatment options.
Cost minimisation and utility are key factors in evaluating fertility treatments, ensuring patients receive effective care without undue financial burden.
Prognostic Factors for IUI Success
Intrauterine insemination (IUI) success rates are influenced by multiple factors, including patient characteristics and specific markers. The effectiveness can vary based on age, health, and previous fertility treatments.
Predictive Markers
Age: Women under 35 typically experience higher pregnancy rates with IUI compared to older patients. Age significantly affects ovarian reserve and egg quality.
Sperm Quality: Sperm count and motility are critical. Higher sperm motility and concentration improve IUI success.
Ovulation Induction: Proper hormonal stimulation is essential. Drugs like clomiphene citrate or gonadotropins can boost ovarian response, enhancing chances of conception.
Cause of Infertility: Specific infertility issues, such as unexplained infertility or mild male factor infertility, respond better to IUI compared to severe cases.
Endometrial Thickness: A thickness of 8-12 mm is ideal for implantation. Thin or excessively thick endometrium can reduce success rates.
Frequently Asked Questions
Costs and expectations for intrauterine insemination (IUI) vary between Saudi Arabia and Kuwait. This section addresses specific questions regarding expenses, success rates, and potential additional fees.
What are the typical expenses involved in intrauterine insemination procedures in Saudi Arabia?
In Saudi Arabia, the cost for a single IUI cycle typically ranges between SAR 3,000 to SAR 7,000. This can vary based on the clinic and additional services required during the procedure.
How does the cost of intrauterine insemination in Kuwait compare to that in Saudi Arabia?
In Kuwait, IUI procedures usually cost between KWD 400 to KWD 800. This range is similar to the pricing in Saudi Arabia when converted, with some centres potentially offering more competitive rates.
What factors contribute to the varying prices of intrauterine insemination in the Middle East?
Several factors influence the price variations including clinic reputation, geographical location, the experience of medical staff, and the inclusion of supplementary services such as medication and follow-up consultations.
How often are IUI treatments successful on the first attempt in Saudi Arabia and Kuwait?
Success rates for IUI on the first attempt in both countries are roughly 10% to 20%. Success depends on individual health factors, age, and the underlying cause of infertility.
What additional fees can be anticipated when undergoing IUI treatments in Saudi Arabia?
Additional costs may include medication, hormone injections, ultrasound monitoring, and laboratory tests. These can add an extra SAR 1,000 to SAR 3,000 to the overall expenses.
Can insurance cover the costs of intrauterine insemination in Kuwait or is it typically an out-of-pocket expense?
In Kuwait, insurance policies generally do not cover IUI procedures, making it an out-of-pocket expense for most patients. It’s advisable to verify with individual insurance providers for specific coverage details.

